The shadow of the Marburg virus has fallen upon Ethiopia, with the confirmation of three deaths, igniting a wave of concern across the region. This outbreak, a serious public health threat, demands immediate attention and action. The situation is evolving rapidly, and understanding the scope of the crisis, the measures being taken, and the potential implications is crucial for both local communities and the international community.
This report delves into the details of the outbreak, including the geographical location, the official responses from the Ethiopian government, and the potential risks to neighboring countries. We will also explore the virus’s transmission, the public health measures being implemented, the symptoms, and the available treatment options. Furthermore, the historical context of Marburg virus outbreaks will be discussed, providing a broader perspective on this deadly disease.
Overview of the Marburg Virus Outbreak in Ethiopia
The recent confirmation of a Marburg virus outbreak in Ethiopia has raised significant public health concerns. This highly contagious and often fatal disease, similar to Ebola, has prompted swift action from health officials and international organizations. The outbreak underscores the importance of rapid response and containment measures to prevent further spread.
Confirmed Deaths and Geographical Location
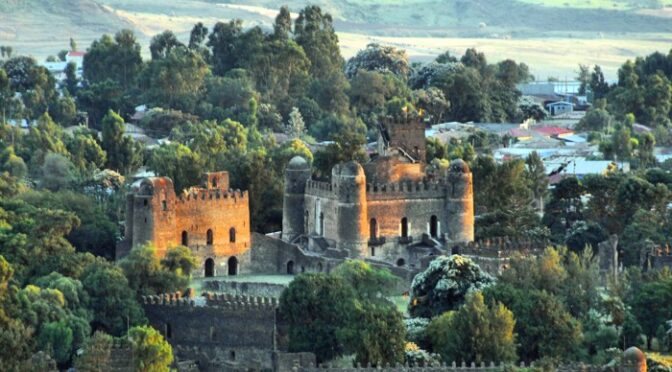
The outbreak has been confirmed with a specific number of fatalities. Understanding the geographical distribution of the virus is crucial for effective containment.The confirmed number of deaths from the Marburg virus outbreak in Ethiopia is three. The outbreak is concentrated in the northwestern part of the country, specifically in the Amhara region. This geographical focus allows for targeted interventions and resource allocation to control the spread within the affected area and prevent it from reaching other regions.
Initial Symptoms of the Marburg Virus
Recognizing the initial symptoms of Marburg virus is essential for early diagnosis and treatment. Early detection significantly increases the chances of survival.The initial symptoms of the Marburg virus often mimic those of other common illnesses, making early diagnosis challenging. These include:
- Sudden onset of fever.
- Severe headache.
- Muscle aches and pains.
- Extreme fatigue.
As the disease progresses, more severe symptoms may develop, such as:
- Diarrhea.
- Abdominal pain.
- Nausea and vomiting.
- Bleeding from various orifices.
Early recognition of these symptoms and immediate medical attention are critical for managing the disease and preventing its spread.
Confirmation of Deaths and Official Responses
The confirmation of deaths from the Marburg virus in Ethiopia has triggered a rapid response from the government and health authorities. This section details the official confirmation of fatalities, the immediate actions taken, and statements released by the Ministry of Health and other relevant bodies. Understanding the official response is crucial for assessing the effectiveness of containment measures and public awareness efforts.
Official Confirmation of Fatalities
The Ethiopian Ministry of Health officially confirmed three deaths related to the Marburg virus outbreak. This confirmation followed laboratory testing and investigations to identify the cause of the illnesses and deaths. The initial reports highlighted the seriousness of the situation, emphasizing the need for swift action to prevent further spread of the virus.
Immediate Government Response
The Ethiopian government’s immediate response to the outbreak included several key actions. These measures were implemented to contain the virus, provide care for those affected, and inform the public about the situation.
- Activation of Emergency Response Teams: The government mobilized emergency response teams, including epidemiologists, healthcare workers, and laboratory specialists, to the affected areas. These teams were tasked with identifying and isolating cases, tracing contacts, and providing medical care.
- Establishment of Isolation Centers: Isolation centers were established to provide specialized care for confirmed and suspected cases of Marburg virus disease. These centers were equipped with the necessary medical supplies and staffed by trained personnel to ensure the safety of patients and prevent further transmission.
- Public Health Education Campaigns: The Ministry of Health launched public health education campaigns to raise awareness about the Marburg virus, its symptoms, and preventive measures. These campaigns utilized various media channels, including radio, television, and social media, to reach a wide audience.
- Contact Tracing Initiatives: Extensive contact tracing efforts were undertaken to identify individuals who may have come into contact with infected persons. These individuals were monitored for symptoms and placed under quarantine if necessary.
Statements from the Ministry of Health and Relevant Authorities
The Ministry of Health and other relevant authorities issued several statements to keep the public informed and provide guidance. These statements aimed to communicate the seriousness of the outbreak, the measures being taken, and the importance of public cooperation.
“The Ministry of Health is working tirelessly to contain the Marburg virus outbreak and protect the health of the public. We urge everyone to follow the guidelines provided by health officials and to seek medical attention if they experience any symptoms.”
These statements also emphasized the importance of:
- Reporting any suspected cases to health authorities immediately.
- Practicing good hygiene, including frequent handwashing and avoiding contact with sick individuals.
- Cooperating with health officials during contact tracing and quarantine procedures.
Regional Alarm and International Implications
The confirmation of Marburg virus deaths in Ethiopia has understandably triggered significant concern across the region and beyond. The highly contagious nature of the virus, coupled with the potential for severe illness and high mortality rates, necessitates a coordinated response to prevent further spread. This section explores the regional impact, international involvement, and potential risks associated with this outbreak.
Neighboring Countries and Regional Concerns
The proximity of Ethiopia to several other nations, combined with cross-border travel and trade, heightens the risk of the Marburg virus spreading beyond its initial confines. This situation has prompted increased vigilance and preparedness measures in neighboring countries.The countries that are directly affected or are expressing heightened concern are:* Sudan: Shares a lengthy border with Ethiopia, and the potential for movement of people and goods makes it a vulnerable neighbor.
Kenya
Also shares a border, increasing the risk of transmission. Kenya has experience with dealing with outbreaks.
Somalia
The ongoing instability and weaker healthcare infrastructure in certain areas may complicate containment efforts.
Djibouti
Is geographically close and could be affected.These countries are likely to be implementing enhanced surveillance, screening at border crossings, and public health campaigns to raise awareness and identify potential cases early.
International Health Organizations’ Involvement
International health organizations play a critical role in supporting Ethiopia’s response to the Marburg virus outbreak. Their expertise, resources, and coordination efforts are essential for controlling the spread of the disease.The organizations involved are:* World Health Organization (WHO): The WHO is typically at the forefront of responding to outbreaks of international concern. They provide technical assistance, guidance, and resources to the affected country.
They also coordinate international efforts to control the outbreak.
Africa Centres for Disease Control and Prevention (Africa CDC)
The Africa CDC is actively involved in supporting African countries in their response to health emergencies. They provide technical expertise, training, and resources to help countries detect, prevent, and control disease outbreaks.
Médecins Sans Frontières (MSF)
MSF often provides direct medical assistance to affected populations, including setting up treatment centers and providing care to patients.
United Nations Agencies
Other UN agencies, such as the United Nations Children’s Fund (UNICEF), may provide support for areas like sanitation, hygiene, and community outreach.These organizations work closely with the Ethiopian Ministry of Health and other national authorities to provide support in areas such as:* Surveillance and Contact Tracing: Identifying and monitoring individuals who have been in contact with infected persons.
Laboratory Testing
Confirming cases and monitoring the spread of the virus.
Treatment and Care
Providing medical care to patients infected with the virus.
Public Health Education
Raising awareness among the public about the virus, its transmission, and preventive measures.
Coordination
Facilitating communication and collaboration among different organizations and stakeholders.
Potential Risks to the Surrounding Region and Beyond
The Marburg virus outbreak poses several potential risks, extending beyond the immediate area of the confirmed cases. Understanding these risks is crucial for developing effective prevention and control strategies.Potential risks include:* Cross-Border Transmission: The movement of people, goods, and animals across borders increases the risk of the virus spreading to neighboring countries. This is particularly concerning given the porous borders and high levels of regional travel.
For example, if a traveler from an infected area unknowingly carries the virus to a major transportation hub like Addis Ababa Bole International Airport, the virus could quickly spread internationally.
Healthcare Worker Infections
Healthcare workers are at high risk of exposure to the virus due to their close contact with infected patients. Inadequate infection control practices in healthcare settings can lead to further spread. During the 2005 Angola Marburg outbreak, numerous healthcare workers were infected.
Community Spread
The virus can spread within communities through contact with infected individuals or contaminated materials. Traditional burial practices, where family members handle the deceased, can also contribute to the spread.
Economic Impact
Outbreaks can disrupt economic activities, leading to loss of productivity, reduced tourism, and trade restrictions. The 2014-2016 Ebola outbreak in West Africa had a devastating economic impact on the affected countries.
International Travel and Trade
The globalized nature of travel and trade increases the risk of the virus spreading to other continents. The virus could be transported by infected travelers to any part of the world, highlighting the need for global surveillance and preparedness.
Strain on Healthcare Systems
Outbreaks can overwhelm healthcare systems, diverting resources and personnel from other essential health services. This can lead to increased mortality rates from both the Marburg virus and other illnesses.
Transmission and Spread of Marburg Virus
Understanding how the Marburg virus spreads is crucial for controlling outbreaks. This section explores the primary modes of transmission, factors influencing its spread within Ethiopia, and examples of how the virus moves from one person to another.
Primary Modes of Transmission
The Marburg virus spreads through several key pathways. Knowledge of these pathways is essential for implementing effective prevention strategies.
- Contact with Infected Animals: The virus’s initial transmission often occurs through contact with fruit bats, the natural reservoir for Marburg virus. This can involve direct contact with the bats themselves or with their bodily fluids, such as saliva, feces, or urine. Hunters or people who work in mines or caves where bats live are at higher risk.
- Direct Contact with Infected Humans: The virus spreads easily from person to person through direct contact with the blood, body fluids (urine, saliva, vomit, etc.), or tissues of an infected person. This includes contact with contaminated objects like needles or bedding.
- Contact with Contaminated Objects: The virus can persist on surfaces and objects, especially in environments where proper hygiene practices are lacking. Touching contaminated surfaces and then touching the mouth, nose, or eyes can lead to infection.
Factors Contributing to Potential Spread Within Ethiopia
Several factors could potentially amplify the spread of the Marburg virus within Ethiopia.
- Limited Healthcare Infrastructure: Weak healthcare systems, particularly in rural areas, can hinder the rapid identification, isolation, and treatment of cases. This can allow the virus to spread more widely before control measures are implemented. Insufficient access to personal protective equipment (PPE) for healthcare workers increases their risk of exposure and further transmission.
- Cultural Practices: Cultural practices, such as traditional burial rituals involving direct contact with the deceased, can facilitate transmission if the deceased died from Marburg virus disease. Additionally, communal living arrangements and close-knit communities can increase the likelihood of exposure.
- Population Movement and Migration: Movement of people within Ethiopia, including migration for work or other reasons, can spread the virus to new areas. This is especially concerning if infected individuals are asymptomatic or have mild symptoms initially, allowing them to travel undetected.
- Poor Hygiene Practices: Lack of access to clean water and sanitation, along with inadequate hygiene practices, can contribute to the spread of the virus. This includes a lack of handwashing with soap and water and improper disposal of medical waste.
Examples of Person-to-Person Spread
The following examples illustrate how the Marburg virus can spread from one person to another.
- Healthcare Settings: A healthcare worker treating a patient with Marburg virus disease who is not wearing appropriate PPE may become infected. The virus can spread through exposure to the patient’s blood or other body fluids during procedures.
- Family Caregivers: Family members caring for a sick individual at home can become infected through direct contact with the patient’s bodily fluids, especially if they are not using protective measures like gloves and masks.
- Burial Practices: During traditional burial ceremonies, individuals who handle the body of someone who died from Marburg virus disease can become infected. This occurs through direct contact with the deceased’s body fluids.
- Sexual Transmission: The virus can persist in semen for several months after recovery. Sexual transmission is possible, even after the initial illness has resolved.
Public Health Measures and Containment Efforts
The Ethiopian government, in collaboration with international health organizations, is implementing a multi-pronged approach to contain the Marburg virus outbreak and prevent further spread. These measures focus on rapid detection, isolation, treatment, and prevention strategies. The success of these efforts hinges on effective communication, community engagement, and resource allocation.
Specific Actions in the Outbreak Response
A coordinated response involves several key actions to manage the outbreak effectively. These actions are designed to control the spread of the virus and protect public health. The following table provides a breakdown of the specific measures:
| Action | Description | Implementation | Goal |
|---|---|---|---|
| Surveillance and Early Detection | Enhanced surveillance systems are in place to identify new cases promptly. This includes active case finding, particularly in high-risk areas. | Healthcare workers are trained to recognize symptoms and report suspected cases immediately. Mobile health teams are deployed to remote areas. | To quickly identify and isolate cases to prevent further transmission. |
| Isolation and Treatment | Patients suspected or confirmed to have Marburg virus are immediately isolated in designated treatment centers. Supportive care is provided. | Isolation units are established with strict infection control protocols. Healthcare workers are provided with personal protective equipment (PPE). | To prevent further spread of the virus and provide the best possible care for infected individuals. |
| Contact Tracing | Identifying and monitoring individuals who have come into contact with confirmed cases is a critical part of the response. | Contact tracing teams are deployed to locate and monitor contacts for 21 days (the incubation period of Marburg virus). Contacts are advised on self-monitoring and quarantine. | To identify and isolate potential new cases before they can transmit the virus. |
| Community Engagement and Awareness | Public health campaigns are being launched to educate the public about the virus, its transmission, and preventive measures. | Information is disseminated through various channels, including radio, television, and community meetings. Emphasis is placed on safe burial practices. | To reduce the risk of transmission by promoting informed behavior and empowering communities to take protective actions. |
Contact Tracing and Quarantine Procedures
Contact tracing is a vital component of controlling the Marburg virus outbreak. It involves systematically identifying individuals who have been exposed to a confirmed case and monitoring them for symptoms. Quarantine is then implemented to limit the spread of the virus.
- Contact Identification: Public health officials use interviews with confirmed cases and their families, as well as review of medical records, to identify all potential contacts. Contacts are categorized based on their level of exposure (high, medium, or low risk).
- Monitoring: Identified contacts are monitored for 21 days, the maximum incubation period for the Marburg virus. This includes daily temperature checks and monitoring for symptoms such as fever, headache, muscle aches, and bleeding.
- Quarantine: Individuals identified as high-risk contacts are placed under quarantine, meaning they are required to remain in a designated location (usually their home) and avoid contact with others. Quarantine is a measure to isolate and observe people who have been exposed to a disease but are not yet ill.
- Testing: If a contact develops symptoms, they are immediately isolated and tested for Marburg virus.
- Support and Communication: Throughout the contact tracing and quarantine process, public health officials provide support and information to contacts. This includes regular communication, access to healthcare if needed, and guidance on how to prevent further spread.
Symptoms, Diagnosis, and Treatment
Understanding the clinical presentation, diagnostic procedures, and available treatment options is crucial for managing Marburg virus disease (MVD). This knowledge is essential for early detection, effective patient care, and controlling the spread of the virus.
Symptoms of Marburg Virus Disease
The symptoms of Marburg virus disease can vary in severity, but they typically manifest in distinct stages. Recognizing these stages is vital for timely diagnosis and intervention.Early-stage symptoms often resemble other common illnesses, making early diagnosis challenging.
- Incubation Period: The incubation period, the time between infection and the onset of symptoms, typically ranges from 2 to 21 days.
- Initial Symptoms: The illness usually begins abruptly with fever, severe headache, and malaise. Other early symptoms include muscle aches (myalgia), and body aches. Gastrointestinal symptoms, such as nausea, vomiting, and diarrhea, may also appear.
Late-stage symptoms become more severe and indicative of organ damage.
- Late-Stage Symptoms: As the disease progresses, patients may experience severe bleeding from various sites, including the nose, gums, and gastrointestinal tract. A rash may develop, often appearing as small, pinpoint red spots (petechiae) or larger areas of bruising (ecchymoses).
- Organ Involvement: Severe cases can lead to organ failure, including liver and kidney damage. Neurological symptoms, such as confusion, irritability, and seizures, may also occur. Patients can also present with jaundice.
- Severity and Mortality: The severity of symptoms varies, and the case fatality rate can range from 24% to 88% depending on the outbreak and supportive care provided.
Diagnosis of Marburg Virus Infection
Accurate and timely diagnosis of Marburg virus infection is critical for effective management and outbreak control. Several diagnostic methods are employed.The diagnosis of Marburg virus infection involves a combination of clinical assessment, laboratory testing, and epidemiological investigation.
- Clinical Assessment: The initial assessment involves evaluating the patient’s symptoms, medical history, and travel history, particularly if the patient has been in an area where Marburg virus is known to occur.
- Laboratory Testing: Several laboratory tests are used to confirm Marburg virus infection. These tests can detect the virus itself or the body’s response to the virus.
- Antibody-capture enzyme-linked immunosorbent assay (ELISA): ELISA tests detect antibodies produced by the body in response to the virus.
- Antigen-capture ELISA: This test detects the presence of viral antigens in the patient’s blood or other body fluids.
- Polymerase chain reaction (PCR): PCR tests can detect the virus’s genetic material (RNA) in blood samples, often providing rapid results.
- Virus Isolation: The virus can be isolated from blood samples in specialized laboratories. This process is time-consuming but can provide definitive confirmation of the infection.
- Sample Collection: Diagnostic samples, such as blood, are collected from patients. Samples must be handled with extreme caution and in a high-containment laboratory due to the high risk of infection.
Treatment and Supportive Care for Marburg Virus Disease
There is no specific antiviral treatment or vaccine available for Marburg virus disease. Treatment focuses on supportive care to manage symptoms and complications.Supportive care is the cornerstone of treatment for Marburg virus disease.
- Fluid and Electrolyte Replacement: Intravenous fluids are administered to maintain hydration and replace lost electrolytes due to vomiting, diarrhea, and bleeding.
- Blood Transfusions: Blood transfusions may be necessary to address blood loss and anemia.
- Pain Management: Medications are given to manage pain, headache, and other symptoms.
- Oxygen Therapy: Oxygen therapy may be provided to patients experiencing respiratory distress.
- Management of Complications: Treatment is provided for specific complications such as bleeding, organ failure, and secondary infections.
- Experimental Therapies: Several experimental treatments, including antiviral drugs and antibody therapies, are being investigated, but none have been proven effective in clinical trials.
- Isolation and Infection Control: Patients are isolated to prevent the spread of the virus. Strict infection control measures, including the use of personal protective equipment (PPE), are implemented to protect healthcare workers and other contacts.
Historical Context of Marburg Virus Outbreaks

Source: ethiopianairlines.com
The emergence of the Marburg virus in Ethiopia necessitates a look back at the history of this deadly disease. Understanding past outbreaks provides crucial context for assessing the current situation, comparing its impact, and highlighting the critical similarities and differences between Marburg and other related viruses like Ebola. This historical perspective is essential for informing public health strategies and improving preparedness.
Past Marburg Outbreaks Globally
The Marburg virus, first recognized in 1967, has a history marked by sporadic outbreaks. These outbreaks have varied in scale and location, but they consistently underscore the virus’s potential for severe disease and high fatality rates.
- 1967: The initial outbreak occurred simultaneously in Marburg and Frankfurt, Germany, and in Belgrade, Serbia. This outbreak, linked to laboratory work with African green monkeys imported from Uganda, resulted in 31 cases and seven deaths. This initial event set the stage for the virus’s identification and the beginning of efforts to understand its transmission and impact.
- 1998-2000: A significant outbreak occurred in the Democratic Republic of Congo (DRC). This outbreak saw 154 cases and a case fatality rate of 83%. This outbreak highlighted the challenges of controlling the virus in resource-limited settings and underscored the need for robust public health infrastructure.
- 2005: An outbreak in Angola was particularly devastating, with 252 cases and 227 deaths, representing a case fatality rate of 90%. This was the largest Marburg outbreak recorded, emphasizing the virus’s potential for rapid spread and high mortality. This outbreak served as a grim reminder of the virus’s threat and the urgency of effective containment measures.
- 2012: An outbreak in Uganda caused 15 confirmed cases and 4 deaths.
- 2017: Uganda reported an outbreak with three confirmed cases and three deaths.
Comparing the Current Outbreak to Previous Ones
Evaluating the current outbreak in Ethiopia against historical data allows for a more informed assessment of its potential impact and the effectiveness of current control measures. Factors like case numbers, fatality rates, geographic spread, and the speed of response are all critical points of comparison.
- Severity and Scope: The current outbreak’s severity is evaluated by the number of confirmed cases, the case fatality rate, and the geographic spread within Ethiopia. Comparing these metrics to past outbreaks, particularly the Angola outbreak of 2005, helps to contextualize the current situation. For instance, if the fatality rate is significantly higher than average, it could indicate a more virulent strain or challenges in providing adequate medical care.
- Geographic Spread: The geographic reach of the current outbreak is also a key factor. If the virus spreads rapidly across multiple regions within Ethiopia or to neighboring countries, it would be a cause for greater concern, similar to the rapid spread seen in some past outbreaks.
- Response Time: The speed and effectiveness of the public health response are critical. This includes early detection, contact tracing, isolation of cases, and the provision of supportive care. The time taken to identify the outbreak, implement control measures, and provide treatment significantly impacts the outbreak’s overall impact. The faster the response, the better the chances of containing the virus.
Differences and Similarities Between Marburg and Ebola Viruses
Marburg and Ebola viruses, both members of the filovirus family, share several characteristics, including their high mortality rates and modes of transmission. However, they also have key differences.
- Similarities:
- Transmission: Both viruses are transmitted through direct contact with infected bodily fluids (blood, saliva, vomit, etc.) and contaminated objects. This mode of transmission makes healthcare settings and close-contact environments particularly vulnerable.
- Symptoms: Both viruses cause similar initial symptoms, including fever, headache, muscle aches, and fatigue, which can make early diagnosis challenging.
- High Mortality: Both viruses are associated with high case fatality rates, often ranging from 23% to 90%, depending on the outbreak and the quality of care provided.
- Differences:
- Genetic Differences: The viruses have distinct genetic structures, which influence their virulence and potential for mutation.
- Geographic Distribution: While both viruses are found in Africa, their geographic distributions and the specific reservoir hosts may vary. Marburg has been linked to fruit bats, while Ebola has been linked to different species.
- Treatment and Vaccines: Currently, there are no approved vaccines or specific treatments for Marburg virus disease, while there are approved vaccines and therapeutics for Ebola.
Challenges and Obstacles in Ethiopia
Ethiopia faces significant hurdles in effectively managing the Marburg virus outbreak. These challenges encompass resource limitations, infrastructural deficiencies, and complexities related to community engagement and awareness. Overcoming these obstacles is crucial for containing the spread of the virus and mitigating its impact on the population.
Resource Constraints
Ethiopia’s healthcare system is often strained, especially in rural areas where outbreaks are more likely to occur. This strain significantly impacts the ability to mount an effective response.
- Limited Diagnostic Capacity: The availability of diagnostic tools, such as PCR tests, is often restricted. This can lead to delays in confirming cases and identifying the scope of the outbreak. The lack of rapid diagnostic capabilities hinders early detection and containment efforts.
- Insufficient Personal Protective Equipment (PPE): Healthcare workers on the front lines are at increased risk due to a shortage of PPE. Adequate supplies of gloves, masks, gowns, and other protective gear are vital to prevent the spread of the virus within healthcare settings.
- Financial Limitations: Securing sufficient funding for outbreak response, including surveillance, contact tracing, treatment, and community outreach, is often a challenge. Resource allocation needs to be prioritized effectively.
Infrastructural Deficiencies
Poor infrastructure further complicates the outbreak response, particularly in remote areas.
- Weak Healthcare Infrastructure: Many rural health facilities lack adequate equipment, trained personnel, and isolation units necessary for managing Marburg virus cases. This limits the capacity to provide proper care and control the spread of the virus.
- Transportation Difficulties: The lack of reliable transportation hinders the rapid transfer of samples to diagnostic centers and the movement of healthcare workers and supplies to affected areas. Poor road conditions and limited access to vehicles exacerbate this issue.
- Communication Challenges: Difficulties in communication, including limited internet access and mobile phone coverage, hamper effective dissemination of information and coordination of response efforts. This impacts the ability to quickly inform the public and healthcare workers about the outbreak.
Community Awareness and Engagement Challenges
Effective community engagement is essential for controlling the spread of the virus, but it faces several obstacles.
- Low Health Literacy: Lack of awareness about the symptoms, transmission, and prevention measures related to Marburg virus can lead to delayed reporting and inadequate adherence to safety protocols. Misinformation and rumors can also undermine trust in public health messages.
- Cultural Practices: Some cultural practices, such as traditional burial rituals, may contribute to the spread of the virus. Addressing these practices requires culturally sensitive communication and engagement.
- Mistrust of Authorities: Mistrust of government or healthcare authorities can hinder cooperation with public health measures. Building trust through transparent communication and community involvement is crucial.
The key challenges for Ethiopia in managing the Marburg virus outbreak include:
- Limited diagnostic and treatment resources.
- Inadequate healthcare infrastructure and transportation.
- Low community awareness and engagement due to low health literacy and cultural factors.
Community Awareness and Public Education

Source: nationsonline.org
Effective community awareness and public education are critical in controlling the Marburg virus outbreak in Ethiopia. A well-informed public is better equipped to recognize symptoms, seek timely medical attention, and adopt preventative measures, thus minimizing the spread of the virus. This section Artikels a comprehensive public health campaign strategy.
Public Health Campaign Design
A multi-pronged public health campaign should be implemented across Ethiopia, utilizing various channels to reach diverse populations. This campaign needs to be culturally sensitive, linguistically appropriate, and tailored to the specific needs of different communities. The campaign should involve collaboration with local leaders, religious figures, community health workers, and media outlets to ensure broad reach and credibility.
Key Messages for the Public
The core messages should be simple, clear, and actionable. They should focus on awareness, prevention, and seeking prompt medical care.
- Understanding Marburg Virus: Explain what Marburg virus is, how it spreads, and the severity of the disease. Emphasize that it is a rare but deadly viral hemorrhagic fever.
- Recognizing Symptoms: Detail the common symptoms of Marburg virus, including fever, headache, muscle aches, fatigue, diarrhea, abdominal pain, and unexplained bleeding.
- Preventative Measures: Provide practical advice on how to prevent the spread of the virus. This includes:
- Avoiding contact with bats and monkeys, as they are known reservoirs of the virus.
- Avoiding contact with the blood or body fluids of infected individuals.
- Practicing safe burial practices.
- Properly disinfecting contaminated surfaces and objects.
- Seeking immediate medical attention if symptoms develop.
- Importance of Early Diagnosis and Treatment: Highlight the importance of seeking medical care immediately if symptoms are present. Early diagnosis and supportive treatment can improve the chances of survival.
- Where to Seek Help: Provide information on where to seek medical care, including local health facilities, hospitals, and emergency contact numbers.
- Debunking Misinformation: Address common misconceptions and rumors about the virus, providing accurate information and dispelling false beliefs.
Educational Materials Examples
A variety of educational materials should be developed and disseminated to reach different segments of the population.
- Posters and Flyers: Visually appealing posters and flyers in multiple languages (Amharic, Oromo, Tigrinya, Somali, etc.) should be displayed in public places like health clinics, markets, schools, and community centers. These should feature clear illustrations and concise messaging about symptoms, prevention, and where to seek help. An example would be a poster illustrating the symptoms of Marburg virus with clear visual representations and easy-to-understand text.
- Radio and Television Announcements: Short, informative radio and television announcements should be broadcast frequently. These announcements should feature trusted voices, such as community leaders or healthcare professionals, delivering key messages in a clear and engaging manner. An example would be a public service announcement (PSA) featuring a well-known local personality explaining the importance of handwashing and avoiding contact with sick individuals.
- Brochures and Fact Sheets: Detailed brochures and fact sheets providing more in-depth information about the virus should be distributed in health facilities and community gatherings. These materials should include illustrations, frequently asked questions (FAQs), and contact information for further assistance. An example is a brochure detailing the incubation period, symptoms, and treatment options for Marburg virus.
- Community Meetings and Workshops: Community health workers and local leaders should organize meetings and workshops to provide information and answer questions. These events can facilitate interactive discussions and address specific concerns within the community.
- Social Media Campaigns: Utilize social media platforms to disseminate information and engage with the public. Create shareable content, including infographics, short videos, and interactive quizzes, to raise awareness and promote preventative measures.
- Training for Healthcare Workers: Healthcare workers require specialized training to effectively manage Marburg virus cases, including proper infection control protocols and patient care.
Future Outlook and Prevention

Source: atcdn.net
The Marburg virus outbreak in Ethiopia presents a serious public health challenge with potential long-term consequences. Addressing these implications and implementing robust preventative measures are crucial to protecting the population and preventing future outbreaks. The focus must be on strengthening healthcare infrastructure, improving surveillance, and fostering community awareness.
Potential Long-Term Implications for Ethiopia
The outbreak’s impact extends beyond the immediate health crisis. It can strain Ethiopia’s already fragile healthcare system, diverting resources and personnel from other essential services. This can lead to increased morbidity and mortality from other diseases. Economic consequences, such as reduced tourism and trade, are also possible, particularly if the outbreak is not contained quickly. Furthermore, the outbreak can erode public trust in government institutions and healthcare providers, hindering future public health efforts.
There is a risk of long-term psychological effects on survivors, healthcare workers, and the wider community, including anxiety and fear.
Recommendations for Preventing Future Outbreaks
Preventing future Marburg virus outbreaks requires a multi-faceted approach. This includes enhancing surveillance systems, improving laboratory capacity, strengthening infection prevention and control practices in healthcare settings, and educating the public about the virus and its transmission. International collaboration and support are essential for providing technical assistance, sharing resources, and coordinating responses. A proactive approach is needed to minimize the impact of future outbreaks.
Preventative Measures
To mitigate the risk of future Marburg virus outbreaks, the following measures are recommended:
- Strengthen Surveillance Systems: Establish and maintain robust surveillance systems to detect and monitor potential outbreaks early. This includes training healthcare workers to recognize symptoms, implementing rapid diagnostic testing, and establishing efficient reporting mechanisms. Early detection is key to controlling the spread.
- Enhance Laboratory Capacity: Improve the capacity of laboratories to diagnose Marburg virus infections quickly and accurately. This involves providing adequate equipment, training laboratory personnel, and ensuring access to appropriate diagnostic reagents and testing protocols. Rapid and accurate diagnosis is critical for effective outbreak response.
- Improve Infection Prevention and Control (IPC) Practices: Implement and enforce strict IPC measures in healthcare facilities. This includes providing healthcare workers with personal protective equipment (PPE), implementing proper hand hygiene protocols, and ensuring safe waste management practices. Proper IPC is vital to prevent the spread of the virus within healthcare settings.
- Promote Community Awareness and Education: Educate the public about the Marburg virus, its transmission, and preventive measures. This includes providing information on avoiding contact with infected individuals and animals, practicing safe burial rituals, and seeking prompt medical attention if symptoms develop. Community engagement is essential for effective outbreak control.
- Strengthen Border Control and Screening: Implement effective screening measures at points of entry, such as airports and border crossings, to identify and isolate individuals who may be infected. This can help prevent the importation of the virus from other affected regions.
- Conduct Research and Development: Support research to develop effective vaccines and treatments for Marburg virus disease. This includes conducting clinical trials, improving diagnostic tools, and exploring potential antiviral therapies. Research is crucial for long-term control and prevention.
- Enhance International Collaboration: Foster collaboration with international organizations, such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), to share information, provide technical assistance, and coordinate outbreak responses. International cooperation is essential for a global response.
- Invest in Healthcare Infrastructure: Strengthen the overall healthcare infrastructure, including hospitals, clinics, and laboratories. This involves providing adequate funding, training healthcare workers, and ensuring access to essential medical supplies and equipment. A strong healthcare system is crucial for responding to outbreaks and protecting public health.
Last Point
In conclusion, the Marburg virus outbreak in Ethiopia is a stark reminder of the constant threat posed by infectious diseases. The confirmed deaths and the regional alarm underscore the need for swift action, effective containment measures, and increased public awareness. While challenges remain, including resource limitations and community awareness, the coordinated efforts of the Ethiopian government, international health organizations, and local communities are essential in managing this crisis and preventing further spread.
The future requires constant vigilance, preparedness, and a commitment to public health to mitigate the impact of future outbreaks.
Top FAQs
What is the Marburg virus?
The Marburg virus is a highly contagious and often fatal hemorrhagic fever virus, similar to Ebola. It causes severe bleeding, organ failure, and can result in death.
How is the Marburg virus transmitted?
The virus is primarily transmitted through contact with infected fruit bats, or bodily fluids of infected people, including blood, vomit, feces, and saliva. Contact with contaminated surfaces and materials also poses a risk.
What are the early symptoms of Marburg virus infection?
Early symptoms include fever, headache, muscle aches, and fatigue. These symptoms can be similar to other illnesses, making early diagnosis challenging.
Is there a cure for Marburg virus?
There is no specific cure for Marburg virus. Treatment focuses on supportive care, such as managing symptoms, providing fluids, and addressing complications. Early supportive care can improve survival rates.
How can I protect myself from the Marburg virus?
Avoid contact with infected individuals and their bodily fluids. Practice good hygiene, including frequent handwashing. Avoid contact with fruit bats and their habitats. If traveling to an affected area, follow health advisories and take necessary precautions.