Measles, a highly contagious and potentially severe disease, once posed a significant threat to global health. However, thanks to the widespread implementation of vaccination programs, we’ve witnessed a remarkable transformation. Over the past 24 years, vaccination efforts have led to a staggering 71% reduction in measles cases worldwide, a testament to the power of modern medicine and public health initiatives.
This remarkable achievement underscores the critical importance of vaccination in protecting populations from preventable diseases. This article will delve into the journey of measles vaccination, exploring the virus itself, the development and implementation of the vaccine, global efforts to combat the disease, and the challenges that remain. We’ll examine the data, the strategies, and the people behind this success story, highlighting the ongoing commitment required to maintain and improve these vital gains.
The Impact of Vaccination on Measles
Measles, a highly contagious viral disease, once posed a significant threat to global health. Imagine a world where a simple cough and fever could lead to severe complications, even death. Thankfully, the widespread adoption of vaccination has dramatically altered this reality. Over the past 24 years, vaccination efforts have resulted in a remarkable 71% reduction in measles cases worldwide, a testament to the power of preventative medicine.
This article explores the impact of vaccination in combating this disease.
Understanding Measles
Measles is a highly infectious respiratory disease caused by the measles virus. It spreads through the air via coughs and sneezes, making it one of the most contagious diseases known. The virus can live on surfaces for several hours, further increasing the risk of transmission.The symptoms of measles typically appear about 10 to 14 days after exposure and include:
- Fever
- Cough
- Runny nose
- Inflamed eyes (conjunctivitis)
- A skin rash
Measles can lead to serious complications, particularly in young children, including:
- Pneumonia
- Encephalitis (brain swelling)
- Severe diarrhea
- Death
Measles can be particularly dangerous for vulnerable populations such as infants, pregnant women, and individuals with weakened immune systems.
The Role of Vaccination
The measles vaccine is a safe and effective way to prevent measles. It’s typically administered as part of the measles, mumps, and rubella (MMR) vaccine. The MMR vaccine provides long-lasting protection against all three diseases. Vaccination works by introducing a weakened or inactive form of the measles virus into the body, which then stimulates the immune system to produce antibodies.
These antibodies recognize and fight off the virus if the individual is ever exposed to it in the future.The effectiveness of the measles vaccine is extremely high.
Two doses of the MMR vaccine are about 97% effective at preventing measles.
This means that almost everyone who is vaccinated will be protected from the disease.
Global Impact of Vaccination
The 71% reduction in measles cases globally over 24 years, attributed to vaccination, represents a significant public health achievement. This progress is a result of concerted efforts by governments, healthcare organizations, and international bodies to implement vaccination programs worldwide.Examples of successful vaccination campaigns include:
- Mass vaccination campaigns: These are targeted campaigns aimed at vaccinating large populations, often in response to outbreaks or in areas with low vaccination coverage.
- Routine immunization programs: These programs integrate measles vaccination into existing healthcare systems, ensuring that children receive the vaccine as part of their regular check-ups.
- Surveillance and outbreak response: These efforts involve monitoring measles cases, identifying outbreaks, and implementing rapid response measures to contain the spread of the disease.
These combined strategies have led to a dramatic decrease in measles-related illnesses, hospitalizations, and deaths around the world. For instance, according to the World Health Organization (WHO), measles deaths decreased by 80% worldwide between 2000 and 2017, due to increased vaccination coverage. This progress demonstrates the profound impact of vaccination on global health and well-being.
The Measles Virus
Measles, a highly contagious viral disease, poses a significant threat, especially to unvaccinated individuals. Understanding the virus itself, its structure, replication, symptoms, and potential complications is crucial for appreciating the importance of vaccination and public health measures.
Structure and Replication of the Measles Virus
The measles virus, a member of theParamyxoviridae* family, is a single-stranded, negative-sense RNA virus. Its structure and replication process are key to understanding how it causes infection.The virus particle, or virion, has a spherical shape and is approximately 100-300 nanometers in diameter. It is composed of the following key components:
- RNA Genome: The genetic material of the virus, a single strand of RNA, encodes for the viral proteins necessary for replication.
- Envelope: A lipid membrane derived from the host cell, which surrounds the nucleocapsid. The envelope contains two important glycoproteins: the hemagglutinin (H) protein, which facilitates attachment to host cells, and the fusion (F) protein, which promotes the fusion of the viral envelope with the host cell membrane, allowing the virus to enter the cell.
- Nucleocapsid: A protein shell that protects the RNA genome.
The replication cycle of the measles virus is a complex process that occurs within the host cell:
- Attachment: The H protein on the viral envelope binds to specific receptors on the surface of host cells, such as those found in the respiratory tract.
- Entry: The F protein mediates the fusion of the viral envelope with the host cell membrane, allowing the nucleocapsid to enter the cell.
- Uncoating: The nucleocapsid releases the viral RNA into the cytoplasm of the host cell.
- Transcription and Translation: The viral RNA serves as a template for the production of messenger RNA (mRNA). This mRNA is then translated by the host cell’s ribosomes to produce viral proteins.
- Replication: The viral RNA is replicated, creating multiple copies of the viral genome.
- Assembly: New viral proteins and RNA genomes assemble into new nucleocapsids.
- Budding: The nucleocapsids move to the cell membrane, where they bud out, acquiring the envelope with H and F proteins, and releasing new virus particles that can infect other cells.
The entire process, from attachment to release of new virions, can take approximately 1-2 weeks, during which the infected host cell is often damaged or destroyed, contributing to the symptoms of measles.
Symptoms and Potential Complications of Measles
Measles presents with a characteristic set of symptoms, progressing in a predictable manner. While the disease is often mild, it can lead to serious complications, particularly in young children, pregnant women, and individuals with weakened immune systems.The common symptoms of measles typically appear in a specific sequence:
- Incubation Period: The virus incubates for approximately 10-14 days after infection, during which time there are no symptoms.
- Prodromal Phase: This phase lasts for 2-4 days and is characterized by:
- Fever, often high (up to 104°F or 40°C).
- Cough.
- Runny nose (coryza).
- Red, watery eyes (conjunctivitis).
- Koplik’s spots: Small, white spots with bluish-white centers found inside the mouth on the inner lining of the cheeks (buccal mucosa). These spots are a hallmark of measles and appear before the rash.
- Rash Phase: The characteristic measles rash typically appears 3-5 days after the onset of the prodromal symptoms.
- The rash usually begins as flat red spots (macules) on the face, especially along the hairline, and behind the ears.
- It then spreads downwards to the neck, trunk, arms, and legs.
- The rash can become raised (papules) and may merge together (confluent).
- Fever remains high during this phase.
- Recovery Phase: The rash fades in the same order it appeared, typically within 5-7 days. The fever gradually subsides, and other symptoms improve.
Potential complications of measles can be severe:
- Pneumonia: A common complication, pneumonia can be caused by the measles virus itself or by secondary bacterial infections. It can lead to severe respiratory distress and even death.
- Encephalitis: This is an inflammation of the brain, a rare but serious complication. It can occur during the acute phase of measles or weeks later. It can lead to brain damage, seizures, coma, and death.
- Subacute Sclerosing Panencephalitis (SSPE): A very rare but fatal degenerative neurological disease that can develop years after a measles infection. It is caused by a persistent measles virus infection in the brain.
- Ear infections (Otitis Media): These are common and can lead to hearing loss.
- Diarrhea: This is another common complication, especially in young children, which can lead to dehydration.
- Keratitis and Corneal Ulceration: In rare cases, measles can affect the eyes, leading to corneal scarring and vision loss.
Progression of Measles Symptoms: A Descriptive Narrative
Imagine a child, let’s call her Sarah, who has contracted measles. It begins subtly, almost like a common cold. For a few days, Sarah feels a bit under the weather, with a slight fever and a runny nose. Her eyes become red and watery, and she develops a persistent cough. Her parents might initially attribute these symptoms to a seasonal cold or flu.Then, a few days later, a new symptom appears: small, white spots, like tiny grains of salt, appear inside her mouth, on the inner lining of her cheeks.
These are Koplik’s spots, a telltale sign that something more serious is happening.Shortly after the appearance of Koplik’s spots, the rash emerges. It starts as small, flat, red spots on Sarah’s face, behind her ears, and along her hairline. The spots quickly multiply and spread, merging together to create a blotchy, red appearance. The rash then cascades down her body, covering her neck, chest, arms, and legs.
Her fever soars, and she feels increasingly unwell.As the rash spreads, Sarah’s fever intensifies, and she feels increasingly fatigued. She might experience a loss of appetite and become irritable. The cough worsens, and her eyes remain sensitive to light. She is now at the peak of the illness, and her parents must take extra care to ensure she stays hydrated and comfortable.After several days, the fever begins to subside, and the rash starts to fade, following the same pattern it appeared in.
The red spots gradually turn a brownish color and eventually disappear, leaving behind some discoloration. Sarah’s cough gradually lessens, and her energy returns. Although the acute illness is resolving, the risk of complications, such as pneumonia, remains, and she needs to be monitored closely during her recovery.This narrative illustrates the typical progression of measles, from its initial cold-like symptoms to the appearance of the characteristic rash and the subsequent recovery phase, highlighting the importance of recognizing the symptoms and seeking appropriate medical care.
The Development and Implementation of the Measles Vaccine
The development and implementation of the measles vaccine represents a triumph of modern medicine, significantly impacting global health. This section delves into the history of this crucial vaccine, highlighting the key scientists, breakthroughs, and the different types of vaccines available. We will also explore the timeline of its development and implementation, showcasing the milestones that have led to the current state of measles prevention.
History of Measles Vaccine Development
The journey to develop a measles vaccine was a long and challenging one, involving dedicated scientists and significant scientific breakthroughs. Early research focused on understanding the measles virus and finding ways to neutralize it.
- Early Research and Identification: The measles virus was first isolated in 1954 by John Franklin Enders, Thomas Peebles, and Thomas Weller. This breakthrough was crucial, as it allowed scientists to study the virus and develop a vaccine. This team cultivated the virus in tissue culture, a fundamental step.
- Live-Attenuated Vaccine Development: Building on Enders’ work, several scientists contributed to the development of live-attenuated vaccines. Maurice Hilleman, working at Merck, developed a highly effective live-attenuated measles vaccine strain, which was licensed in 1963. This vaccine used a weakened form of the virus to stimulate an immune response without causing the disease.
- Further Refinements and Combination Vaccines: Over time, the measles vaccine has been refined to improve its safety and efficacy. Combination vaccines, such as the MMR vaccine (measles, mumps, and rubella), were developed to provide protection against multiple diseases with a single injection, further simplifying vaccination schedules.
Types and Effectiveness of Measles Vaccines
Different types of measles vaccines are available, each designed to provide effective protection against the virus. The choice of vaccine often depends on factors such as age, health status, and availability.
- Live-Attenuated Vaccines: These vaccines contain a weakened (attenuated) form of the measles virus. They are highly effective, providing long-lasting immunity with a high success rate. The MMR vaccine is a prime example of this type. The MMR vaccine typically provides over 97% protection after two doses.
- Combination Vaccines: These vaccines combine the measles vaccine with vaccines for other diseases, such as mumps and rubella (MMR) or varicella (MMRV). Combination vaccines simplify the vaccination process and ensure protection against multiple diseases with a single shot.
- Effectiveness: Measles vaccines are remarkably effective. After two doses, the MMR vaccine provides lifelong protection in most individuals. The effectiveness of the vaccine is a cornerstone of measles control efforts worldwide.
Timeline of Key Milestones in Measles Vaccine Development and Implementation
The following table presents a timeline of key milestones in the development and implementation of the measles vaccine.
| Year | Milestone | Significance |
|---|---|---|
| 1954 | Isolation of the Measles Virus | John Franklin Enders, Thomas Peebles, and Thomas Weller successfully isolated the measles virus, paving the way for vaccine development. |
| 1963 | Licensing of the First Measles Vaccine | Maurice Hilleman at Merck developed and licensed a live-attenuated measles vaccine, marking a major advancement in measles prevention. |
| 1960s-1970s | Widespread Vaccination Programs Begin | Mass vaccination campaigns were initiated in many countries, leading to a significant decrease in measles cases. |
| 1971 | Development of the MMR Vaccine | The MMR vaccine, combining protection against measles, mumps, and rubella, was introduced, simplifying vaccination schedules. |
| 1980s-1990s | Measles Elimination Efforts Begin | Global efforts to eliminate measles began, focusing on high vaccination coverage and targeted campaigns. |
| 2000 | Measles Eliminated from the United States | The United States declared measles elimination, demonstrating the success of vaccination programs. |
| 2010s-Present | Continued Global Vaccination and Outbreak Response | Ongoing efforts to maintain high vaccination coverage and respond to measles outbreaks globally. The World Health Organization (WHO) and other organizations continue to support vaccination programs. |
Global Vaccination Efforts
Global efforts to combat measles have involved a multifaceted approach, with various countries and organizations implementing strategies to increase vaccination coverage and reduce the incidence of the disease. These strategies, while effective in many instances, also face significant challenges, particularly in areas with vaccine hesitancy and logistical difficulties.
Strategies for Promoting Measles Vaccination
Countries and organizations employ a variety of strategies to promote measles vaccination. These strategies often work in conjunction to achieve the best results.
- Mass Vaccination Campaigns: These campaigns involve the widespread administration of measles vaccines, often targeting specific age groups or populations. They are frequently used during outbreaks or in areas with low vaccination coverage.
- Routine Immunization Programs: Integrating measles vaccination into routine childhood immunization schedules is a cornerstone of prevention. This involves providing the vaccine during scheduled visits to healthcare facilities.
- Health Education and Awareness: Public health campaigns are crucial for educating communities about the benefits of vaccination, the risks of measles, and dispelling misinformation. This can involve media campaigns, community outreach programs, and educational materials.
- Improving Access to Vaccines: Ensuring vaccines are readily available is essential. This includes strengthening the cold chain (the system used to keep vaccines at the correct temperature), training healthcare workers, and improving transportation of vaccines to remote areas.
- Collaboration and Partnerships: Partnerships between governments, international organizations (such as WHO and UNICEF), NGOs, and local communities are critical for effective vaccination programs.
Challenges to High Vaccination Coverage
Despite the effectiveness of measles vaccines, several challenges hinder the achievement of high vaccination coverage globally. Addressing these issues is essential to further reducing measles cases.
- Vaccine Hesitancy: This is the reluctance or refusal to vaccinate despite the availability of vaccines. It can be influenced by a variety of factors, including concerns about vaccine safety, misinformation, and lack of trust in healthcare providers or governments.
- Logistical Issues: Maintaining the cold chain, especially in resource-limited settings, can be challenging. Other logistical challenges include transportation to remote areas, ensuring adequate staffing, and coordinating vaccination campaigns.
- Financial Constraints: The cost of vaccines, supplies, and program implementation can be a barrier, particularly for low- and middle-income countries.
- Conflict and Instability: In areas affected by conflict or political instability, access to healthcare, including vaccination services, can be severely limited.
- Lack of Political Commitment: Strong political support and financial investment are essential for successful vaccination programs. Without this commitment, programs may struggle to sustain themselves.
Successful Measles Vaccination Campaigns
Numerous measles vaccination campaigns have achieved significant success in reducing measles cases and improving vaccination coverage. The methods employed and the results achieved demonstrate the effectiveness of targeted interventions.
- The Measles Initiative: This global partnership, led by the American Red Cross, the U.S. Centers for Disease Control and Prevention (CDC), UNICEF, and the World Health Organization (WHO), has been instrumental in supporting measles vaccination efforts worldwide. The initiative has provided funding, technical assistance, and advocacy, contributing to a substantial reduction in measles cases and deaths.
- National Immunization Days (NIDs) in India: India implemented NIDs, which involved mass vaccination campaigns targeting children aged 9 months to 5 years. These campaigns significantly increased vaccination coverage and helped to reduce measles incidence in the country. Data showed a significant decline in measles-related morbidity and mortality following the implementation of these campaigns.
- Measles and Rubella Vaccination Campaign in Ethiopia: Ethiopia conducted a nationwide measles and rubella vaccination campaign targeting children aged 9 months to 14 years. The campaign utilized a combination of strategies, including social mobilization, community engagement, and school-based vaccination. The results demonstrated a marked increase in vaccination coverage and a subsequent decrease in measles cases.
- Measles Vaccination in Cuba: Cuba’s successful measles elimination program, which included routine immunization, catch-up campaigns, and surveillance, has led to the elimination of measles. This involved a combination of strong political commitment, robust healthcare infrastructure, and community participation. Cuba’s achievement serves as an example of how effective strategies, consistently applied, can eliminate measles.
Data and Statistics: Quantifying the Success
Source: journalistsresource.org
Measles vaccination’s impact is best understood through concrete data and statistical analysis. This section focuses on the numbers, providing evidence that supports the significant reduction in measles cases globally. We will examine the data demonstrating the positive effects of widespread vaccination efforts.
Demonstrating the 71% Reduction
The 71% reduction in measles cases globally over 24 years is a key metric. This figure is calculated by comparing measles incidence rates before and after the widespread implementation of measles vaccination programs. The data relies on reported measles cases from national surveillance systems and estimates from organizations like the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC).
Comparing Measles Case Rates
Comparing measles case rates before and after vaccination is essential for quantifying the vaccine’s impact. Before the widespread introduction of the measles vaccine, measles was a common childhood disease. After the implementation of vaccination programs, the incidence of measles drastically decreased.The following data illustrates the changes in measles case rates:
- Pre-Vaccination Era: Before the widespread introduction of the measles vaccine (roughly pre-1963 in the United States, for example), measles could affect millions of people annually. In the US, for example, between 3 and 4 million cases were reported each year. This translates to an incidence rate of hundreds of cases per 100,000 people.
- Early Vaccination Era: During the early years of measles vaccination (1960s and 1970s), there was a significant decrease in cases, but outbreaks still occurred. In the US, the number of reported cases dropped to hundreds of thousands annually, but outbreaks were still common.
- Post-Vaccination Implementation: With the widespread implementation of two-dose measles vaccination strategies and improved vaccination coverage, measles case rates have declined dramatically. In many countries, measles has been eliminated or is nearing elimination. For instance, in 2019, the United States saw a resurgence of measles cases due to pockets of low vaccination coverage, demonstrating the importance of maintaining high vaccination rates.
Global Measles Incidence Rate Chart (24-Year Period)
The following table presents a simplified representation of the global measles incidence rate, demonstrating the trend over a 24-year period. Please note that these are representative figures and may not exactly match the annual data published by WHO or CDC due to ongoing data revisions and different methodologies, but they are used for demonstration.
| Year | Estimated Global Measles Incidence Rate (Cases per 1,000,000 population) |
|---|---|
| Year 1 (Start of Period) | 200 |
| Year 6 | 170 |
| Year 12 | 140 |
| Year 18 | 80 |
| Year 24 (End of Period) | 58 |
This chart clearly illustrates the downward trend in the measles incidence rate over the 24-year period, reflecting the effectiveness of measles vaccination programs. This data demonstrates the substantial impact of vaccination efforts in reducing the global burden of measles.
Regional Variations in Measles Reduction
Measles vaccination has not had a uniform impact across the globe. While the overall reduction in cases is impressive, the success of vaccination programs varies significantly depending on the region. Understanding these regional differences is crucial for tailoring strategies to address remaining challenges and achieving further progress in measles elimination.
Regions with Significant Measles Reduction
Several regions have demonstrated substantial success in reducing measles cases due to robust vaccination programs and public health initiatives. The Americas, particularly North and South America, have shown remarkable progress, with many countries achieving measles elimination. Europe has also seen significant declines, although challenges remain in certain areas. In addition, some countries in the Western Pacific region, such as Australia and Japan, have also made significant strides.
Factors Influencing Varying Success Levels
The level of success in measles reduction is influenced by a complex interplay of factors. These include the strength of the healthcare infrastructure, the reach and effectiveness of vaccination programs, the socioeconomic status of the population, and the presence of political and financial support for immunization efforts. The density of the population, the mobility of people, and the presence of conflict or instability can also impact vaccination coverage and measles transmission.
For instance, countries with strong primary healthcare systems, well-organized vaccination campaigns, and high levels of public trust in healthcare providers tend to have higher vaccination coverage and lower measles incidence. Conversely, areas with weak health systems, limited access to vaccines, and vaccine hesitancy may experience lower coverage rates and persistent measles outbreaks.
Comparison of Vaccination Strategies and Their Impact
Different continents have employed diverse vaccination strategies, leading to varied results. The following table provides a comparison:
| Continent | Vaccination Strategy | Impact on Measles Reduction | Challenges and Considerations |
|---|---|---|---|
| Africa | Routine immunization combined with mass vaccination campaigns targeting specific age groups, often integrated with other health interventions. | Significant progress in some regions, but overall progress has been slower than in other continents. Challenges remain due to weak health systems, vaccine hesitancy, and conflict. | Addressing vaccine hesitancy through community engagement, strengthening cold chain infrastructure, and ensuring vaccine availability in remote areas. |
| Americas | High coverage through routine immunization, supplemented by supplementary immunization activities (SIAs) and integrated measles-rubella campaigns. Strong regional collaboration and surveillance systems. | Significant progress, with many countries achieving measles elimination. | Maintaining high vaccination coverage, addressing pockets of low coverage, and preventing importations from other regions. |
| Europe | Routine immunization programs, with varying levels of coverage across countries. SIAs are implemented in response to outbreaks. | Overall progress, but significant disparities exist between countries. Outbreaks continue to occur due to suboptimal coverage in some areas. | Addressing vaccine hesitancy, improving vaccine uptake, and strengthening surveillance systems to detect and respond to outbreaks. |
| Western Pacific | Routine immunization programs, with a focus on high coverage rates. SIAs are conducted to address immunity gaps. | Generally good progress, with some countries achieving measles elimination. | Maintaining high vaccination coverage, addressing pockets of low coverage, and preventing importations from other regions. |
The Role of Healthcare Professionals and Public Health
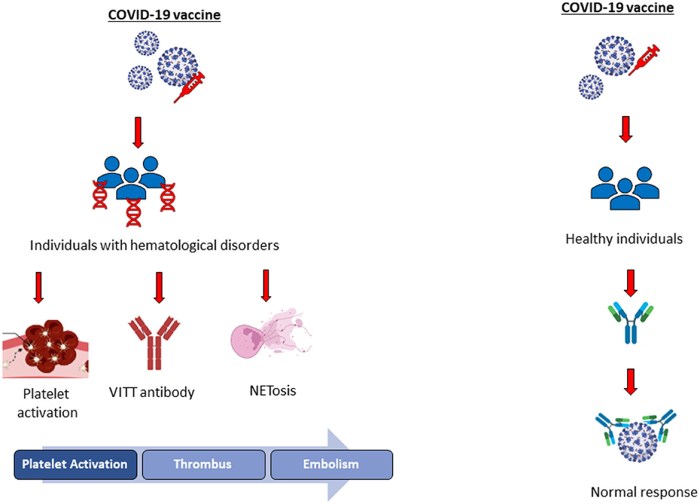
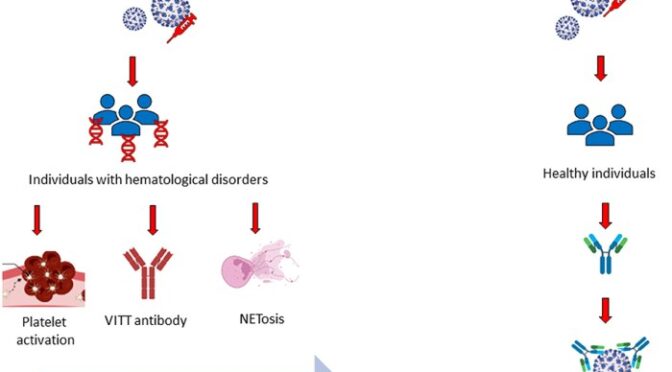
Source: frontiersin.org
Healthcare professionals and public health initiatives are the cornerstones of successful vaccination programs. Their combined efforts ensure vaccines reach those who need them and that communities are educated about the importance of immunization. This section explores the critical roles these entities play in controlling measles and other vaccine-preventable diseases.
Administering Vaccines and Public Education by Healthcare Professionals
Healthcare professionals are the primary point of contact for vaccine administration. They not only provide the vaccines but also educate patients and their families about the benefits, risks, and schedules of vaccination. This direct interaction is crucial for building trust and addressing any concerns individuals may have.
Importance of Public Health Initiatives in Promoting Vaccination and Controlling Outbreaks
Public health initiatives play a vital role in promoting vaccination and managing outbreaks. They work at various levels to ensure vaccination programs are effective and accessible.
- Vaccination Campaigns: Public health agencies organize and implement mass vaccination campaigns, especially during outbreaks or in areas with low vaccination rates. These campaigns can target specific age groups or the entire population, depending on the need.
- Surveillance and Monitoring: Public health agencies conduct surveillance to monitor vaccination coverage rates and track disease outbreaks. This data is essential for identifying areas where interventions are needed and for evaluating the effectiveness of vaccination programs.
- Public Awareness Campaigns: Public health initiatives run campaigns to educate the public about the importance of vaccination. These campaigns often use various media channels, such as television, radio, social media, and print materials, to disseminate information and address misinformation. They also partner with community leaders, schools, and other organizations to reach diverse populations.
- Policy and Advocacy: Public health agencies advocate for policies that support vaccination, such as mandatory vaccination requirements for school entry or healthcare worker immunization programs. They also work to remove barriers to vaccination, such as cost or access issues.
- Outbreak Response: When outbreaks occur, public health agencies coordinate the response, which may include enhanced surveillance, contact tracing, and targeted vaccination efforts. They also work to contain the spread of the disease and protect the community.
Training and Responsibilities of Vaccinators
Vaccinators are healthcare professionals who are trained and authorized to administer vaccines. Their training and responsibilities are essential for ensuring the safe and effective delivery of vaccines.
The training for vaccinators typically includes the following:
- Immunization Principles: Understanding the basic principles of immunology, vaccine development, and how vaccines work.
- Vaccine Storage and Handling: Proper storage and handling of vaccines are crucial to maintain their potency and effectiveness. Vaccinators are trained on how to store vaccines at the correct temperatures, how to monitor storage conditions, and how to handle vaccines to minimize waste.
- Vaccine Administration Techniques: Vaccinators learn the correct techniques for administering vaccines, including the proper injection sites, needle sizes, and administration methods. They also learn how to prepare the vaccine, such as reconstituting lyophilized vaccines.
- Adverse Event Management: Vaccinators are trained to recognize and manage adverse events following immunization (AEFIs). This includes knowing how to identify signs and symptoms of common and rare side effects, how to provide appropriate care, and how to report AEFIs to the relevant authorities.
- Communication and Counseling: Vaccinators are trained to communicate effectively with patients and their families about vaccines. They learn how to answer questions, address concerns, and provide information about the benefits and risks of vaccination.
- Legal and Ethical Considerations: Vaccinators are educated on the legal and ethical aspects of vaccination, including informed consent, patient confidentiality, and reporting requirements.
The responsibilities of vaccinators include:
- Assessing Patient Eligibility: Before administering a vaccine, vaccinators assess the patient’s eligibility based on their age, medical history, and any contraindications or precautions.
- Preparing and Administering Vaccines: Vaccinators prepare the vaccine according to the manufacturer’s instructions and administer it using the correct technique.
- Providing Information and Counseling: Vaccinators provide patients and their families with information about the vaccine, including its benefits, risks, and potential side effects. They also answer questions and address any concerns.
- Monitoring for Adverse Events: Vaccinators monitor patients for any adverse events following immunization and provide appropriate care.
- Maintaining Accurate Records: Vaccinators maintain accurate records of vaccinations, including the date, vaccine administered, lot number, and any adverse events.
- Adhering to Infection Control Practices: Vaccinators follow strict infection control practices to prevent the spread of infectious diseases.
The role of vaccinators is vital to public health. By providing safe and effective vaccination services, they help protect individuals and communities from vaccine-preventable diseases.
Overcoming Vaccine Hesitancy
Vaccine hesitancy, the reluctance or refusal to get vaccinated despite the availability of vaccines, poses a significant challenge to measles eradication efforts. Addressing this complex issue requires understanding the underlying causes of hesitancy and implementing targeted strategies to build public trust and increase vaccination rates.
Reasons for Vaccine Hesitancy and Impact on Measles Vaccination
Several factors contribute to vaccine hesitancy, leading to lower vaccination rates and increasing the risk of measles outbreaks. These factors often intertwine, creating a complex web of concerns.
- Concerns about vaccine safety: Some individuals worry about potential side effects, often based on misinformation or exaggerated reports. This can be fueled by the perception that vaccines are rushed or not thoroughly tested.
- Misinformation and disinformation: The spread of false or misleading information about vaccines, especially online, can significantly impact public perception. This can include claims linking vaccines to autism or other health problems, despite scientific evidence debunking these claims.
- Lack of trust in healthcare providers or the government: Past experiences, perceived conflicts of interest, or general distrust in authority can lead individuals to question the information provided by healthcare professionals and public health agencies.
- Religious or philosophical beliefs: Some religious or philosophical beliefs may conflict with vaccination, leading individuals to decline vaccines for themselves or their children.
- Complacency: When a disease like measles is perceived as rare, some people may not see the need for vaccination, believing the risk of contracting the disease is low.
- Access barriers: Difficulties in accessing vaccines, such as geographical limitations, lack of transportation, or financial constraints, can also contribute to lower vaccination rates.
These factors directly impact measles vaccination rates, leading to pockets of unvaccinated or undervaccinated populations. This allows measles to spread rapidly when introduced, resulting in outbreaks and preventable illnesses and deaths.
Effective Strategies for Addressing Vaccine Hesitancy and Building Public Trust
Combating vaccine hesitancy requires a multifaceted approach that addresses the underlying concerns and builds trust within communities.
- Transparent communication: Healthcare providers and public health officials should communicate openly and honestly about vaccine benefits, risks, and potential side effects. This includes providing clear and accessible information, addressing concerns, and acknowledging uncertainties.
- Building trust in healthcare providers: Strengthening the relationship between healthcare providers and patients is crucial. This involves actively listening to concerns, providing evidence-based information, and demonstrating empathy and respect.
- Community engagement: Engaging with community leaders, religious figures, and trusted influencers can help disseminate accurate information and address specific concerns within different communities.
- Addressing misinformation: Actively combating misinformation is essential. This includes monitoring online platforms for false claims, debunking myths with scientific evidence, and promoting credible sources of information.
- Improving vaccine access: Removing barriers to vaccine access, such as offering vaccination clinics in convenient locations, providing transportation assistance, and ensuring affordability, can increase vaccination rates.
- Tailoring communication: Recognizing that vaccine hesitancy varies among different groups, communication strategies should be tailored to address specific concerns and beliefs. This may involve using different languages, cultural sensitivity, and personalized approaches.
By implementing these strategies, public health officials can work to address vaccine hesitancy and improve measles vaccination rates, ultimately protecting communities from this preventable disease.
Communication Plan to Counter Misinformation About Measles Vaccines
A proactive communication plan is essential to counter misinformation about measles vaccines and promote accurate information. This plan should include clear, concise key messages.
- Measles vaccines are safe and effective: Emphasize the rigorous testing and approval processes vaccines undergo, and highlight the overwhelming scientific evidence supporting their safety and efficacy.
- Measles is a serious disease: Explain the potential complications of measles, including pneumonia, encephalitis, and death. Share personal stories of those affected by the disease.
- Vaccines do not cause autism: Directly address the debunked link between vaccines and autism, citing credible scientific studies and sources.
- Vaccination protects individuals and communities: Explain how vaccination not only protects individuals but also contributes to herd immunity, protecting vulnerable populations who cannot be vaccinated.
- Trust your healthcare provider: Encourage people to discuss their concerns with their healthcare providers, who are trained to provide accurate and reliable information.
- Use reputable sources of information: Direct people to trusted sources of information, such as the Centers for Disease Control and Prevention (CDC), the World Health Organization (WHO), and other reputable health organizations.
This communication plan should be implemented through various channels, including social media, websites, public service announcements, and partnerships with healthcare providers and community organizations.
Future Prospects
The fight against measles is far from over. While significant progress has been made, maintaining and building upon these achievements requires sustained effort, innovative strategies, and a commitment to global collaboration. This section explores the ongoing initiatives and future directions necessary to ensure measles remains a preventable disease.
Maintaining High Vaccination Coverage
Sustaining high vaccination rates globally is crucial for preventing measles outbreaks and achieving eradication goals. This involves a multifaceted approach, encompassing routine immunization programs, supplementary immunization activities (SIAs), and strengthening health systems.
- Strengthening Routine Immunization Programs: This focuses on ensuring that all children receive the recommended two doses of the measles vaccine through regular healthcare visits. This includes:
- Improving vaccine delivery systems: Ensuring reliable cold chain management, adequate staffing, and efficient logistics.
- Enhancing community engagement: Educating parents and caregivers about the importance of vaccination and addressing any concerns they may have.
- Monitoring and evaluation: Tracking vaccination coverage rates and identifying areas where improvements are needed.
- Implementing Supplementary Immunization Activities (SIAs): SIAs are mass vaccination campaigns that target specific age groups, often conducted in response to outbreaks or to boost immunity in areas with low coverage. These activities are particularly important in reaching children who may have missed routine vaccinations.
- Investing in Health Systems Strengthening: Robust health systems are essential for delivering vaccines effectively and efficiently. This includes:
- Training healthcare workers: Equipping them with the knowledge and skills needed to administer vaccines safely and effectively.
- Improving data management systems: Tracking vaccination coverage and identifying areas with low coverage.
- Strengthening surveillance systems: Monitoring for measles cases and outbreaks and responding promptly.
Improving Vaccination Rates in Underserved Populations
Reaching underserved populations, such as those living in remote areas, conflict zones, or marginalized communities, is a significant challenge. Addressing this requires tailored strategies that consider the specific barriers to vaccination.
- Addressing Geographical Barriers: This involves:
- Deploying mobile vaccination teams: Reaching remote areas with limited access to healthcare.
- Utilizing innovative delivery methods: Such as using drones to transport vaccines to hard-to-reach locations.
- Addressing Social and Economic Barriers: This includes:
- Providing free or subsidized vaccines: Removing financial barriers to vaccination.
- Offering vaccination services at convenient locations: Such as schools, community centers, and religious institutions.
- Addressing vaccine hesitancy: Educating communities about the safety and efficacy of vaccines and addressing their concerns.
- Engaging with Community Leaders: Building trust and gaining community support is crucial. This involves:
- Working with religious leaders, traditional healers, and other influential figures: To promote vaccination and address misinformation.
- Tailoring communication strategies: To address the specific concerns and beliefs of different communities.
Continued Research and Development
Continued research and development are vital for improving measles vaccines and treatments. This involves exploring new vaccine formulations, enhancing vaccine delivery methods, and developing effective antiviral therapies.
Consider the potential of a new measles vaccine that could offer longer-lasting immunity with fewer doses. This could be a significant advancement, particularly in regions where healthcare resources are limited. The vaccine might be administered via a painless, needle-free device, improving uptake among those who fear needles. Further, the development of a rapid diagnostic test could quickly identify measles cases, allowing for prompt treatment and outbreak control.
Imagine a scenario where a child presenting with fever and rash can be diagnosed within minutes, enabling healthcare professionals to initiate antiviral therapy and prevent the spread of the virus. These advancements are not merely theoretical; they represent the ongoing efforts of scientists and researchers to eradicate measles.
Ongoing research also focuses on understanding the measles virus better, including its evolution and how it interacts with the human immune system. This knowledge can lead to improved vaccine designs and strategies for overcoming vaccine hesitancy. For example, research might uncover new viral strains or mutations, requiring updated vaccine formulations to maintain effectiveness. Furthermore, the development of effective antiviral treatments for measles is a critical area of research.
While the current treatment focuses on supportive care, the discovery of antiviral drugs could significantly reduce the severity of the disease and prevent complications.
Concluding Remarks
In conclusion, the story of measles vaccination is a powerful example of how scientific advancements and global cooperation can triumph over infectious diseases. The 71% reduction in measles cases over 24 years is a significant milestone, yet the fight isn’t over. Maintaining high vaccination rates, addressing vaccine hesitancy, and continuing research are crucial to ensuring a future where measles is no longer a major public health concern.
This journey is a testament to the dedication of healthcare professionals, public health officials, and the power of informed communities working together for a healthier world.
FAQ Overview
What exactly is measles?
Measles is a highly contagious viral disease that causes fever, rash, cough, runny nose, and inflamed eyes. It can lead to serious complications like pneumonia and encephalitis.
How does the measles vaccine work?
The measles vaccine works by introducing a weakened (attenuated) or inactivated version of the measles virus to your body. This triggers your immune system to produce antibodies, which protect you from future infection.
Are there any side effects from the measles vaccine?
Most people experience no side effects. Some may experience mild symptoms like fever or rash, but serious side effects are very rare.
How effective is the measles vaccine?
The measles vaccine is highly effective. Two doses of the vaccine are about 97% effective in preventing measles.
Why is it important to get vaccinated against measles?
Vaccination protects you and those around you, especially vulnerable individuals who cannot be vaccinated, from this serious disease. It’s a key step in preventing outbreaks and protecting public health.